Recent Headlines
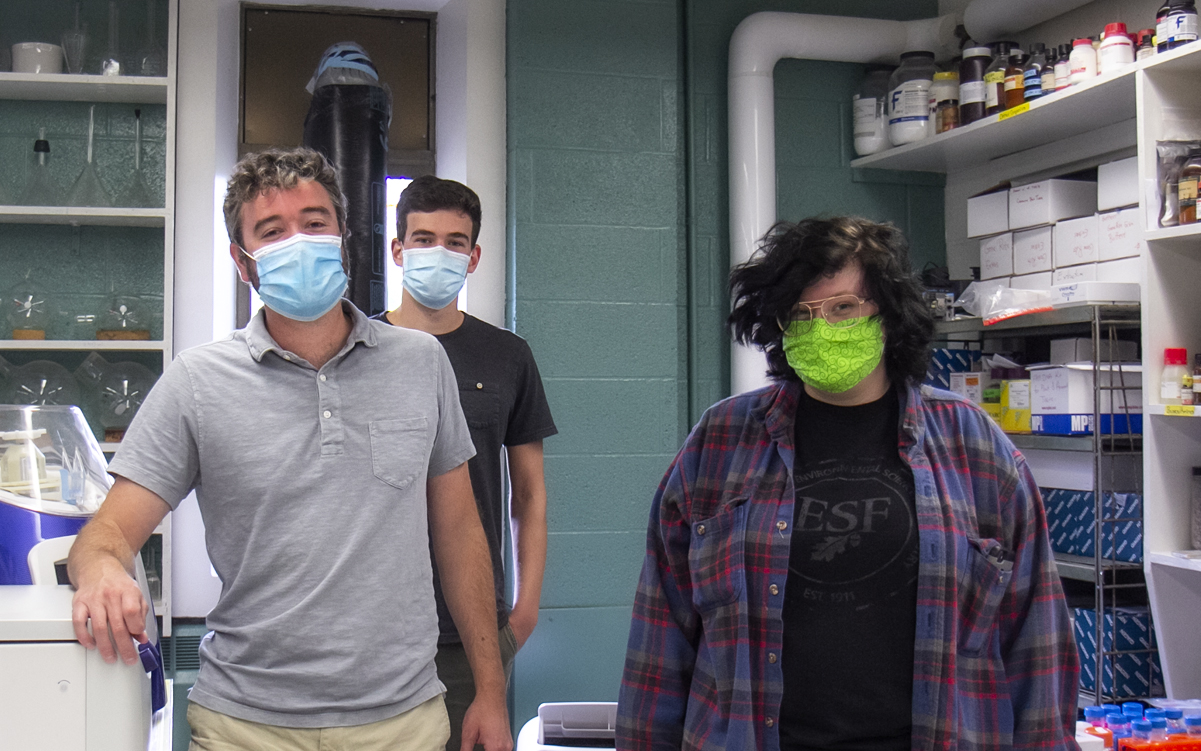
From left: Ariana Fenty, Dr. Hyatt Green, and Maxwell Wilder. Green and his research team monitor the presence of SARS-CcV-2 RNA in wastewater, the virus that causes COVID-19, alerting the state and participating cities to increase and decrease in viral transmission.
ESF Researchers at Forefront of SARS-CoV2 Monitoring
Dr. Hyatt Green likens the ultracentrifugal process to detect SARS-CoV-2 RNA in wastewater to a salad spinner.
"In a salad spinner you put the lettuce in, spin it fast and the water comes off the lettuce," said Green. "We're doing the same thing with the wastewater, but it's the SARS-CoV-2 RNA that sinks to the bottom of the tube."
As part of the SARS-CoV-2 Early Warning Wastewater Surveillance Platform (SARS2-EWSP), Green and his research team, monitor the presence of SARS-CoV-2 RNA in wastewater, the virus that causes COVID-19, alerting the state and participating cities to increases and decreases in viral transmission. These real-time trends provide critical information for reopening and closing decisions.
In the SARS2-EWSP, the tubes are spun at 150,000 times the force of gravity. "It's a tremendous amount of force that concentrates and purifies the viral RNA at the bottom of the tube," explained Green.
Green and his research team - Ariana Fenty, lab technician ('20), and Maxwell Wilder, a Ph.D. student - began developing the method in April after being contacted by Dr. David Larsen, an epidemiologist at Syracuse University, who wondered if recent success monitoring wastewater in the Netherlands could be replicated in Central New York.
Green joined forces with Dr. Frank Middleton at Upstate Medical University and started taking samples from Onondaga County's main wastewater facility.
"We had some initial difficulties finding the supplies to detect the RNA from wastewater," said Green, "so we had to develop a new method based on ultracentrifugation."
In addition to spinning the wastewater sample at high speeds, the team uses a concentrated sucrose solution that further purifies the RNA while it's being concentrated. A provisional patent has been filed on this process.
The New York State Department of Health (DOH) selected the SARS2-EWSP to pilot a statewide coronavirus transmission early warning system. With $500,000 in state pilot funding, the project will expand into Albany, Newburgh and Buffalo, and increase the frequency of surveillance in Onondaga County.
Once fully operational, the early warning system will enable these municipalities to better track increases and decreases in coronavirus transmission and make more informed decisions regarding reopening and closing businesses and schools.
"We're analyzing wastewater from 11 different counties across New York state," Green said, "running about 200 samples a day" with assistance from Quadrant Biosciences Inc. Green's lab continues to do research and development on the analytical techniques. "It's not just about SARS-CoV-2," said Green. "We're very interested in seeing how these analytical techniques and wastewater surveillance, in general, can be used to monitor other pathogens and monitor potential future pandemics."
Green credits his team, who worked tirelessly in the lab at Upstate Medical University, with the success of the project. "It was really brave on their part," said Green. "This was in mid-April at the height of the pandemic and they were coming into the lab using their knowledge and skills in molecular biology to do what they could to help fight the pandemic."
Currently, Green's team is seeing a lot of negative results which corresponds with the low number of cases in Onondaga County.
"When we started analyzing samples in late April we were detecting it quite often in the wastewater at moderately high concentrations, but as cases started to decline locally, we also saw that same decline in wastewater," he said.
Because they are continually monitoring the wastewater from Onondaga County's five wastewater treatment plants, Green is confident they would see an uptick there in their results about a week before it was seen in community testing.
"And that week-lead time is very valuable from a public health standpoint," he said.